
70% smaller stomach without cuts. How? Meet ESG.
Obesity treatment has evolved dramatically over the past few decades. Not long ago, weight loss surgery meant large incisions and prolonged recovery. The introduction of minimally invasive techniques – first laparoscopic “keyhole” surgeries and now endoscopic procedures – has transformed bariatric care. Today, patients seeking significant weight loss without surgery have a groundbreaking option: Endoscopic Sleeve Gastroplasty (ESG), a non-surgical procedure that shrinks the stomach from within. This article explains what ESG is, how it works as an endoscopic weight loss method, how it compares to traditional bariatric surgeries, and why it’s generating excitement as a non-invasive obesity treatment for eligible patients.
A New Era in Bariatric Treatment: From Surgery to Endoscopy
Bariatric surgery has always aimed to reduce stomach capacity and curb hunger, but the methods have become progressively less invasive. Traditional gastric bypass and sleeve gastrectomy are highly effective for weight loss but involve surgical incisions and permanent alterations to anatomy. Over time, surgeons developed advanced laparoscopic techniques – even “scarless” approaches like the Bikini Line gastric sleeve where incisions are hidden at the bikini line – to minimize trauma. Now the frontier has moved to endoscopic therapies performed entirely through the mouth. This evolution means that for the first time, patients can achieve meaningful weight loss without any external cuts or scars. Endoscopic Sleeve Gastroplasty is at the forefront of this new era, offering a less invasive alternative for those who need help losing weight but are hesitant about surgery.
What is Endoscopic Sleeve Gastroplasty (ESG)?
Endoscopic Sleeve Gastroplasty is a modern bariatric procedure that uses an endoscope (a flexible tube with a camera and tools) to reduce the stomach’s size without surgical removal of tissue. In ESG, the doctor inserts the endoscope through the patient’s mouth into the stomach and uses a special suturing device to place stitches in the stomach wall. These sutures cinch the stomach into a smaller, tube-like shape, effectively creating a “sleeve” internally. Unlike a surgical sleeve gastrectomy, no portion of the stomach is cut out; instead, the stomach is folded in on itself and sewn to greatly reduce its volume (by roughly 70–80% of its original capacity). This smaller stomach can hold much less food, so patients feel full faster and eat dramatically smaller portions, leading to weight loss. Importantly, ESG does not reroute the intestines or involve any abdominal incisions, making it a truly incision-free procedure.
Endoscopic Sleeve Gastroplasty is performed through the mouth using a flexible endoscope equipped with a suturing system. In ESG, the endoscope (black tube in the illustration) is advanced into the stomach to place a series of stitches (blue) along the stomach’s inner lining. These sutures fold and tighten the stomach, reducing its volume and shaping it into a narrow sleeve. The right panel shows the stomach after ESG, with a much smaller, tube-like shape that restricts food intake. Because ESG is done endoscopically, there are no external cuts or scars, and the stomach anatomy remains intact (no parts removed).
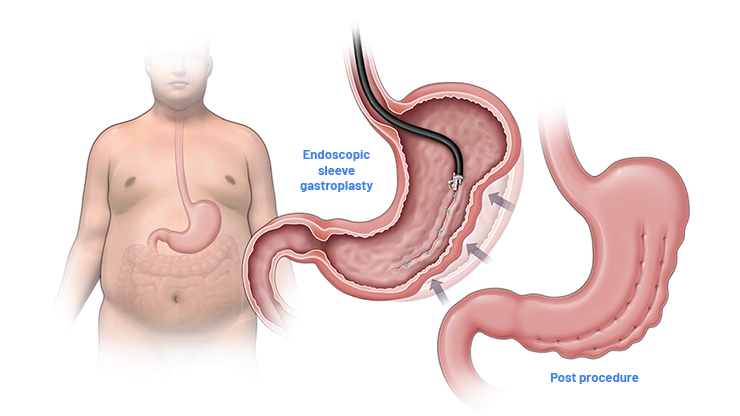
Stomach configuration before and after the ESG
ESG vs. Traditional Bariatric Surgery (Gastric Bypass or Sleeve)
How does ESG compare to surgical options like a gastric bypass or laparoscopic sleeve gastrectomy? The biggest difference is invasiveness. ESG is non-surgical – it’s done via endoscope, so there are no abdominal incisions, no scars, and no surgical wounds to heal. Traditional procedures like sleeve gastrectomy or Roux-en-Y gastric bypass require several incisions in the abdomen (even if done laparoscopically) and permanently alter the stomach or digestive tract. In a gastric bypass, surgeons create a small stomach pouch and reroute the small intestine, and in a sleeve gastrectomy about 75–80% of the stomach is surgically removed. These operations generally produce major weight loss, but they come with higher surgical risks, a few days of hospitalization, and longer recovery periods measured in weeks.
By contrast, ESG is much less invasive. There’s no cutting or stapling of organs – the stomach is shrunk from the inside with stitches. The entire ESG procedure typically takes about 60–90 minutes under general anesthesia, and patients usually go home the same day (or after an overnight observation). Recovery is faster and easier: most people resume normal daily activities within 2–3 days, versus a couple of weeks or more after surgery. ESG also preserves the natural anatomy and function of the stomach – food still follows the normal route and all digestive organs remain intact. This means a lower risk of nutritional deficiencies; unlike bypass patients, ESG patients usually do not require lifelong vitamin supplementation for malabsorption issues.
Another key difference is that ESG is adjustable and reversible if needed. Stitches can theoretically be removed or tightened in follow-up endoscopic sessions (for example, to re-tighten the sleeve if some dilation occurs, or to reverse the procedure), whereas surgical sleeve or bypass are permanent changes. Furthermore, because ESG doesn’t involve abdominal cutting, it doesn’t leave any visible scars and tends to have a lower rate of serious complications. According to a leading clinical trial, the rate of serious adverse events with ESG is around 2%, which is markedly lower than typical rates seen with surgical bariatric procedures. In short, ESG offers a middle ground: it achieves significant weight loss but with substantially less risk and downtime, making it an attractive option for patients who want to lose weight without surgery.
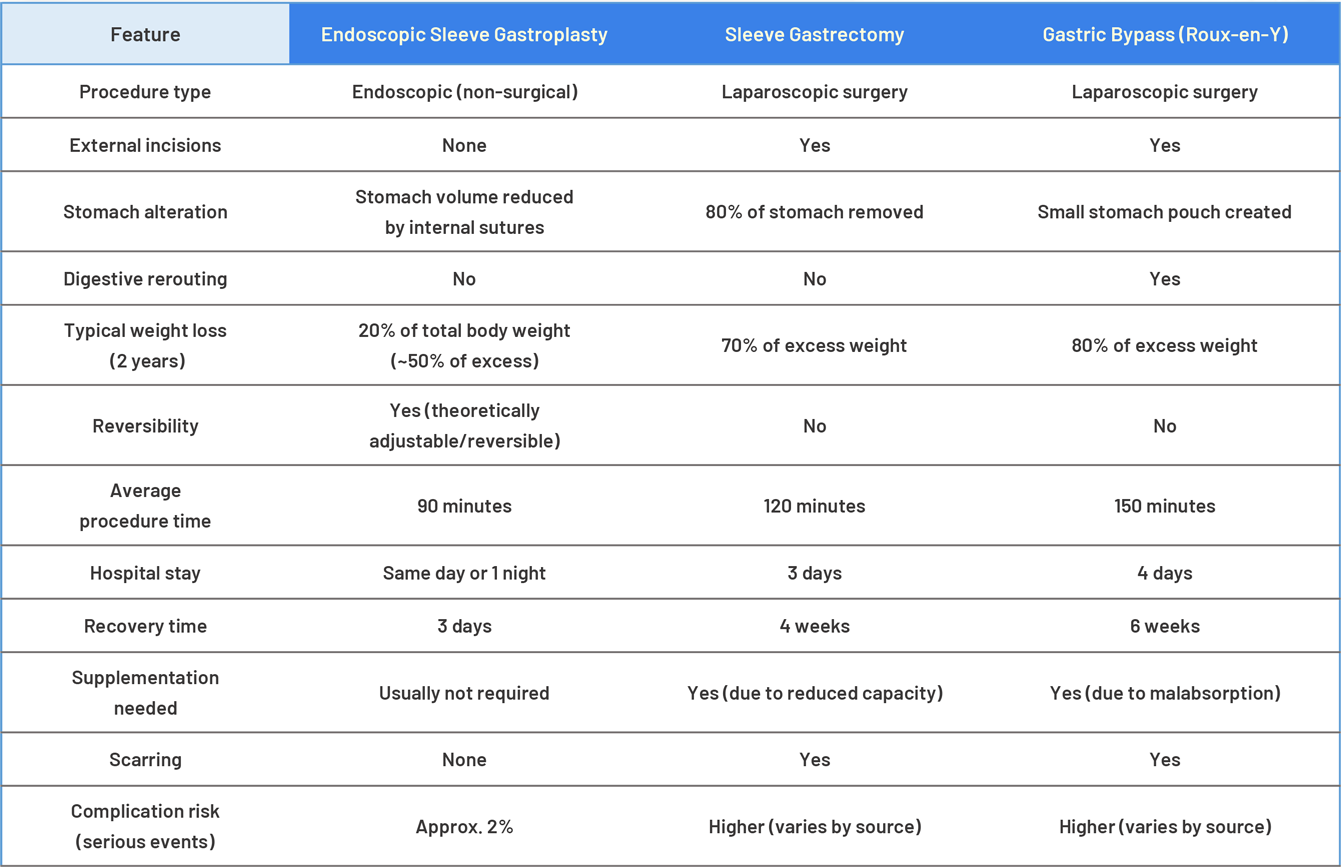
That said, traditional surgeries still have their place. Procedures like gastric bypass or surgical sleeve can yield greater total weight loss and may be more appropriate for patients with higher BMI or severe obesity-related illnesses. On average, surgical patients often lose a larger percentage of their excess body weight (for example, gastric bypass patients might lose ~60–80% of excess weight, and sleeve gastrectomy ~50–70% excess weight over 1–2 years). ESG typically results in a more moderate weight loss – we’ll discuss the results next – so extremely obese patients (BMI 50+, for instance) or those needing a very rapid, major weight reduction might still be steered toward surgery. However, for many people in the low to mid obesity range, the trade-off of slightly less weight loss for a far safer, less invasive procedure is well worth it.
Benefits of ESG: Why Patients Are Embracing Endoscopic Weight Loss
ESG’s growing popularity is driven by a number of patient-friendly benefits. Here are some of the top advantages of Endoscopic Sleeve Gastroplasty:
-
Minimally Invasive (No Cuts or Scars): ESG requires no external incisions. The entire procedure is done through the mouth, so patients are left with zero scars on the abdomen. This incision-free approach means less post-procedure pain and no wound healing issues. For many who fear surgery, knowing there’s no “going under the knife” is a major relief.
-
Quick Recovery & Short Hospital Stay: Because there’s no surgical wound, recovery is rapid. Most ESG patients are up and walking shortly after the procedure and can return to normal daily activities within a couple of days. In fact, ESG is often an outpatient or same-day procedure, meaning you can go home the same day (some providers keep patients overnight for observation, but no prolonged hospital stay is needed). Comparatively, traditional surgery patients may spend 2–3 days in the hospital and require 2–4 weeks before resuming work or exercise.
-
Lower Risk and Safe Profile: Avoiding major surgery generally lowers the risk of complications. ESG has no risk of wound infections or hernias at incision sites (since there are none). Serious complications like bleeding or perforation are rare (about 2%, as noted) and are typically managed without open surgery. Global medical communities have recognized ESG’s safety – for example, the International Federation for the Surgery of Obesity’s Bariatric Endoscopy Committee endorses ESG as a safe and effective obesity treatment. Likewise, the UK’s National Institute for Health and Care Excellence (NICE) assessed ESG and found it “safe in the short and long-term when combined with lifestyle changes,” recommending it as an effective option for eligible patients.
-
No Stomach Resection & Preserved Anatomy: Unlike a surgical sleeve or bypass, ESG does not remove any part of the stomach or reroute intestines. The stomach’s anatomy and digestion function remain normal. This means ESG patients generally avoid the malabsorption issues and strict vitamin supplementation requirements that can come with gastric bypass. The pylorus (the stomach’s outlet valve) is untouched, so food continues to pass naturally into the intestines – just in smaller quantities. Many patients appreciate that ESG is organ-sparing and preserves future options (since the stomach is still intact, one could later choose a surgical procedure if needed).
-
Effective Weight Loss: While ESG’s results may not quite match a gastric bypass, it still produces significant weight loss for most patients. By reducing stomach volume by roughly 75% and slowing gastric emptying, ESG helps people feel full on small meals and dramatically lowers calorie intake. Clinical studies have shown meaningful outcomes – on average, patients lose around 13–20% of their total body weight in the first year after ESG. For example, one major trial reported ESG patients lost 13.6% of body weight by 12 months on average, which equated to about 49% of their excess weight lost in a year. This level of weight reduction can significantly improve or resolve obesity-related conditions (diabetes, hypertension, sleep apnea, etc.) in many cases. And because ESG is typically combined with a supervised diet and lifestyle program, patients often see improvements in overall health and habits alongside the weight loss.
-
Reversible and Repeatable if Needed: ESG is unique in that it can be adjusted over time. If a patient does not achieve the desired result, or if some weight is regained after a couple of years, a repeat endoscopic tightening (sometimes called a “re-sleeve”) can be done to refresh the restriction. In extreme cases, the sutures can be removed endoscopically to restore the original stomach, meaning the procedure is considered reversible. This flexibility gives patients and doctors more options in long-term management, whereas an irreversible surgical sleeve or bypass cannot be easily modified.
All these benefits make ESG an appealing choice, especially for individuals who want weight loss without surgery or who have concerns about the risks and lifestyle changes associated with surgical procedures. But who exactly is ESG best suited for? We’ll cover that next.
Is ESG Safe and Effective? What the Research Shows
ESG is a relatively new procedure (first performed in the mid-2010s), but a growing body of evidence supports its safety and effectiveness. Over 40,000 ESG procedures have already been performed worldwide, and thousands of patients have been studied in clinical trials and follow-up studies. The data show that ESG can lead to substantial weight loss and health improvements when combined with dietary and lifestyle changes – albeit a bit less weight loss than the more aggressive surgeries. Most patients lose between 10% and 20% of their starting body weight within a year of the procedure, and can maintain a large portion of that loss in subsequent years with proper follow-up. For instance, the landmark MERIT randomized trial found patients who underwent ESG lost about 49% of their excess weight by 12 months, and 68% of those patients maintained most of that weight loss at the 2-year mark. These outcomes were vastly better than diet and lifestyle alone in the trial, underscoring that ESG offers a real clinical benefit, not just a placebo effect.
Crucially, ESG has demonstrated a strong safety profile. Published studies and global health authorities report that serious complications are uncommon. In the MERIT trial, the rate of serious adverse events was ~2%. The types of complications that can occur (though rare) include bleeding from a suture site or an accidental perforation of the stomach, which in most cases can be repaired endoscopically. There have been no procedure-related deaths reported in the major ESG studies. Most patients experience some short-lived side effects such as a sore throat (from the endoscope), nausea, cramps, or abdominal pain for a few days post-procedure – these are typically managed with medication and oral fluids. Because ESG is less traumatic to the body, the overall stress and inflammation is lower than in surgery, leading to quicker recovery and fewer risks like blood clots or respiratory issues post-op.
 Dr Donatas Danys, our bariatric surgeon and PhD, participating in ESG training (Madrid, Spain)
Dr Donatas Danys, our bariatric surgeon and PhD, participating in ESG training (Madrid, Spain)
The long-term durability of ESG is also promising but still being studied. We now have 5-year follow-ups in some reports, and many patients have maintained a significant portion of their weight loss. However, as with any weight loss method, individual results vary and regaining weight is possible if one does not adhere to healthy eating and lifestyle changes. ESG should be viewed as a tool to facilitate weight loss, and its success long-term hinges on the patient’s commitment to diet, exercise, and possibly adjunct therapies (such as behavioral counseling). The good news is that by significantly jump-starting weight loss and inducing early satiety, ESG often helps patients build momentum and healthier habits that can sustain them for the long run. And with endorsements from organizations like IFSO and the American Society for Gastrointestinal Endoscopy (ASGE) recognizing ESG as a valid treatment, patients and providers can feel confident that this procedure is evidence-based and not merely experimental.
Who Is a Candidate for ESG (and Who Isn’t)?
Endoscopic Sleeve Gastroplasty is designed for people who are overweight or obese and need help achieving weight loss, but who either do not qualify for bariatric surgery or prefer to avoid surgery. Typically, candidates for ESG have a Body Mass Index (BMI) of 30 or higher. This includes the category of Class I obesity (BMI 30–34.9) who normally wouldn’t be eligible for surgical bariatric procedures, as well as Class II (BMI 35–39.9) and even Class III (BMI 40+ in some cases). In fact, experts note that ESG is particularly beneficial for patients with BMI in the 30–40 range – it can help these individuals lose a significant amount of weight without resorting to an operation. It’s also an option for higher-BMI patients (BMI 40–50 or more) who cannot undergo surgery due to medical risk or who strongly wish to try a less invasive approach first. That said, super-obese patients might achieve only modest results with ESG alone; often, they will be counseled that ESG can be a bridge therapy (to lose some weight and improve health before a possible future surgery) or that multiple treatments may be needed.
You might consider ESG if you:
-
Have a BMI of ≥30 (generally between 30 and ~45 for best results) and have struggled to lose weight through diet and exercise alone.
-
Do not qualify for bariatric surgery or don’t want it. Perhaps your BMI isn’t high enough under standard guidelines for surgery, or you have health conditions that make surgery risky, or you simply want to avoid an operation and permanent anatomical changes.
-
Are motivated to make lifestyle changes. ESG works best when coupled with a healthy diet, exercise, and behavior change. It’s ideal for patients willing to follow medical guidance on nutrition and activity after the procedure to maximize and maintain their weight loss.
-
Have obesity-related health issues (like diabetes, high blood pressure, sleep apnea) that could improve with weight loss – but again, you prefer a less invasive treatment option at least as a first step.
-
Have not had prior stomach surgery. ESG is usually done in patients who have not had a previous gastric bypass or sleeve. Prior surgeries can alter anatomy or cause scar tissue that might make ESG technically difficult. (However, ESG can sometimes be used as a revision for weight regain after a surgical sleeve, by tightening the stomach again endoscopically – this is a special scenario to discuss with a specialist.)
On the other hand, ESG would not be appropriate for:
-
Patients with certain hiatal hernias or gastrointestinal conditions that require surgery.
-
Those who need to lose weight extremely rapidly for an urgent medical reason (surgery might be more direct in some cases).
-
Individuals unwilling to commit to the necessary diet and lifestyle modifications post-procedure – ESG is a tool, not a magic bullet, and it can be undone by poor habits if one isn’t careful.
If you’re considering non-invasive obesity treatment options, it’s crucial to consult with qualified bariatric specialists. They can explain the pros and cons of ESG vs. other treatments in the context of your personal health profile. In the hands of an experienced practitioner like Dr. Donatas Danys, PhD – a bariatric surgeon known for embracing innovation safely – you can be confident that treatments like Endoscopic Sleeve Gastroplasty are administered with the highest standards of care. With the combination of medical progress and expert guidance, achieving meaningful weight loss without traditional surgery is an attainable goal, opening a new pathway for those seeking a healthier future.
How much does Endoscopic Sleeve Gastroplasty cost?
We’ve prepared a dedicated page where you can find the full cost of Endoscopic Sleeve Gastroplasty, along with everything that’s included in the package. You’ll also find detailed information about how the trip is organised, what to expect before and after the procedure, and how to prepare. Click here.
Interested in bariatric topics in general? We’ve put together a playlist of videos to help you understand the procedures, recovery, and real patient journeys here: